Your cart is currently empty!
Author: digital
-

ACORN UK Celebrates 10 Years of Organizing at National Conference in Leeds, Marking Victories and Continuing Advocacy.
ACORN UK hosted their national UK conference in Leeds, with more than 200 ACORN delegates from more than 30 attendants across the UK in attendance! Members celebrated wins, including a recent action where four hundred members had successfully beaten back TSB bank requirements for mandatory rent increases, and ACORN UK’s ten year anniversary of collective organizing! Of course, the actions continued, with ACORN Bristol advocating for a member to be able to stay in their home after the city council rejected their right of succession. The good work continues!
-

ACORN Canada Celebrates 20 Years of Organizing and Demands National Tenant Rights at 7th Biennial Convention.
ACORN Canada celebrated 20 years of community organizing at their 7th Biennial National Convention in Oshawa, with over 250 members attending from coast to coast! Members marched to the CMHC office in Toronto to deliver 300+ tenant testimonials and demand that the Renters Bill of Rights set National Tenant Rights Standards.
-

ACORN Kenya Champions Clean Environment in Korogocho: A Major Win for Public Health.
In June, ACORN Kenya mobilized a major action protecting residents in Korogocho, Nairobi’s largest slum. Korogocho doesn’t have a designated garbage site, creating massive public health issues, including sickness and blocked drains, which has contributed to deadly flooding. ACORN leaders Asha Abdi and Halima Osman led a crowd confronting the Ward Manager’s office, securing a meeting and commitments to support the campaign. Mazingira Safi Ni Haki Yetu! A Clean Environment is Our Right!
-

Welcome Solidarjetà Malta: A New Ally in the Fight Against Worker Exploitation!
ACORN International is thrilled to welcome Solidarjeta Malta into the fold! Solidarjetà is a Maltese non-partisan Trade and Tenant union looking to end the exploitation of workers by organizing and uniting all workers regardless of gender, race, ethnic origin, religion, class, marital status, sexual orientation, gender identity, age, disability, or caring responsibilities.
-

Justicitiz-ACORN Liberia: Unstoppable in Campaign Against Socfin Group for Civil Rights and Environmental Oversight
Justicitiz-ACORN Liberia continued their incredible campaign against palm oil and rubber giant Socfin Group, after forcing the corporation to fix a draining ditch that was flooding a village last year, and the demands of their open letter demanding increased civil rights and environmental oversight from Socfin Group’s shady activities. When the people stand together, we are unstoppable!
-

Riverains Ensemble: Championing Health and Truth Against Political Misinformation on Pesticides
The Riverains Ensemble continues to organize tirelessly for victims of pesticides near industrial farming operations. They are a major source of advocacy and information countering the misinformation campaign of politicians like Jordan Bordella, who claim to be on the side of the people, while actually attempting to relax regulations on pesticides, causing major health concerns for working people.
-

ACORN Honduras’ April Initiatives: Fostering Collaboration and Growth
In April, ACORN Honduras hosted numerous meeting sessions for their members, alongside training and planning sessions with partner organizations. Their efforts focused on fostering collaboration and growth within the community.
-

ACORN Peru’s April Efforts: Supporting Mothers and Empowering Members
In April, ACORN Peru was hard at work collecting and distributing food baskets for Mother’s Day, while also organizing multiple training sessions for their members. Their dedication to supporting the community and empowering individuals is truly inspiring.
-

Living Rent’s April Wins: Standing Together for Member Rights
Living Rent had several wins for their members in April, including for new Living Rent Castlemilk members Hiwa and Kharman, who have spent two years in a substandard apartment, including no boiler, a collapsed ceiling, black mould, and a landlord unwilling to address any of it. Living Rent sprang into action, and immediately got the boiler fixed, and are pressuring the landlord to fix the ceiling and address the mould. When we stand together, we win!
-
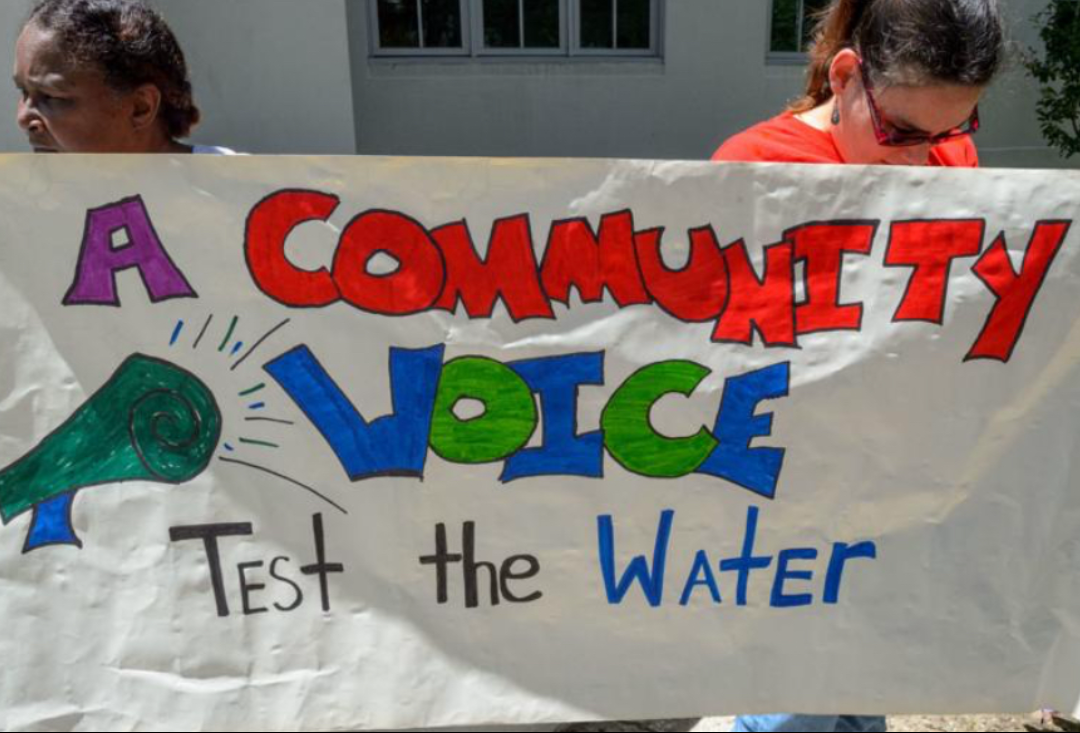
A Community Voice Champions Lead Testing in New Orleans
A Community Voice advocated for increased lead testing in the water and soil in New Orleans, a public health issue that continues to disproportionately affect our POC population, the working class, and children.
